Tackle the three biggest challenges to your nursing program’s enrollment growth
My colleagues and I have fielded about 400 university requests for nursing program research over the years. While our research finds strong employer and student demand for these programs, we’ve also heard concern and frustration from leaders of nursing programs around the country. Over 60% of baccalaureate programs struggle to recruit faculty, and nursing programs at all levels struggle to secure clinical placements for their students, meaning your program likely faces significant barriers to long-term enrollment growth.
-
80,000+
nursing applications rejected in 2022 due to capacity limits.
Get the numbers on the nursing shortage
As leaders of nursing programs know all too well, the COVID-19 pandemic added strain to an already dangerous nursing deficit in the United States. Low wages, long hours, and physical and emotional strain coupled with an aging population have all contributed to a nationwide nursing shortage present since the 1990s. The National Center for Health Workforce Analysis anticipates a shortage of 1 million nurses by the end of 2030.
Increased student interest in nursing programs suggests an easy solution for this deficit— production of more nurses—but the capacity limits discussed below prevent expansion.
Our Professional and Adult Education Advisory Services researchers have spent the last few months exploring the hurdles facing nursing programs and the strategies our partners are using to help mitigate these capacity challenges.
1. Partner with healthcare providers to alleviate faculty shortage in near-term
Nursing accreditation bodies require strict student-to-faculty ratios, straining programs at all degree levels as the nationwide faculty pool shrinks. Three factors drive this shortage:
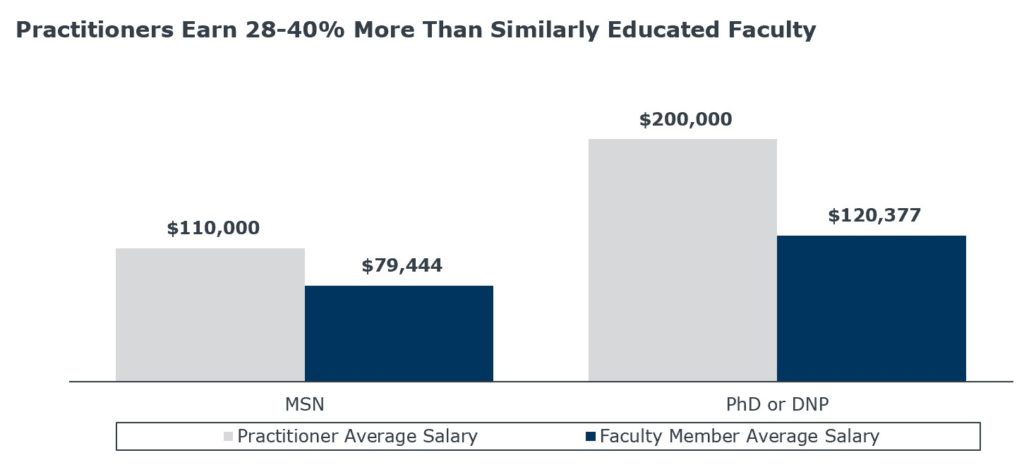
- A sizeable pay gap between academic and practice jobs (as illustrated in the chart below),
- High retirement rates among existing faculty, and
- A poor student understanding of the faculty role, making them unlikely to pursue educator careers.
Two practices emerged across our research to respond to the faculty shortage: academic-practice partnerships and “growing” existing students into future faculty members.
Academic-practice partnerships mitigate salary discrepancies
Academic-practice partnerships can take two forms:Full-time clinical practitioner reassignment: Regional health care provider-partners assign practitioners to teach full-time while paying them at practice rates. This has a couple of benefits:
- Negates academic-practice salary discrepancies.
- Benefits both institutions and health care providers, who expand their nurse pipeline and will have an opportunity to recruit nurses directly from the student pool.
Part-time clinical practitioner partnership: Practitioners teach on a part-time basis while being paid at faculty rates, lowering health care partners’ commitment. Part-time clinical practitioner partnerships:
- Reduces salary discrepancies between practitioners and faculty members
- Offer practitioners improved work-life balance through fewer clinical shifts.
A “grow your own faculty” approach provides a long-term solution, but requires time and investment.
Tackle the faculty shortage at its root by cultivating full-time faculty from your own student body. This three-pronged approach consists of:
- Targeting and supporting talented students with an aptitude for teaching or research.
- Ensuring motivated students receive funding to support graduate-level education, whether through institutional scholarships or federal funding (e.g., the HRSA Nurse Faculty Loan Repayment Program).
- Committing to hiring graduates into the faculty ranks. Nursing leadership, however, note they’re careful to balance “home-grown” faculty alongside external hires to maintain diversity of thought and background on campus.
2. Increase nonmonetary preceptor incentives and support to address clinical placement shortage
Nursing students at all degree levels must complete clinical hours to earn an accredited degree. But a shortage of clinical preceptors makes this requirement increasingly difficult. The preceptor challenge is greatest at the graduate level, as the American Association of Colleges of Nursing (AACN) requires supervision of master’s-level nursing students at a 1:1 ratio.
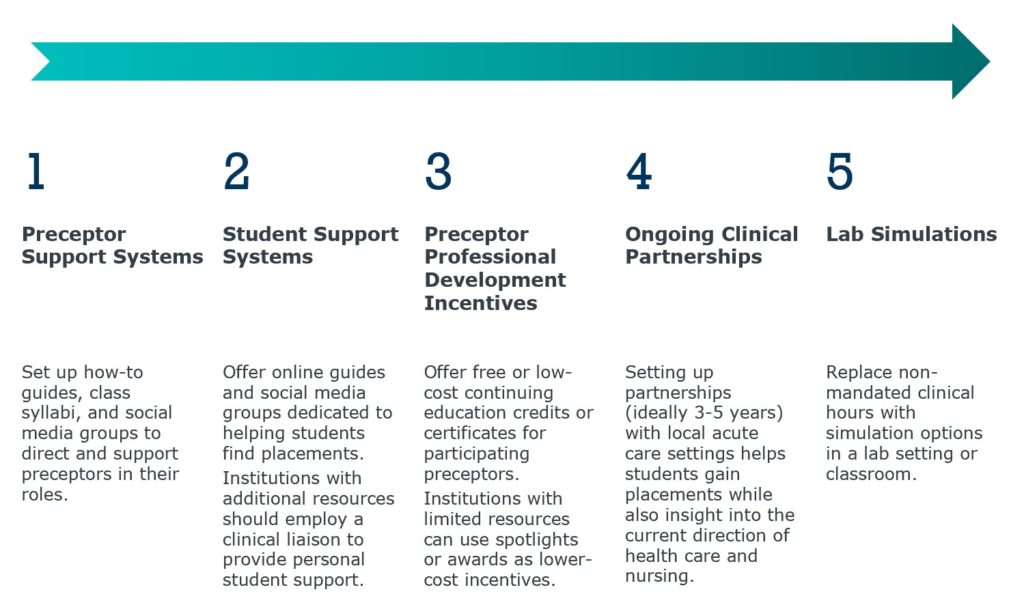
Lack of pay and high competition makes finding preceptors increasingly difficult. 90% of US schools do not pay nursing preceptors, forcing nursing programs to rely on the small pool of working professionals willing to take on mentees with no financial compensation. Additionally, other health professions such as physician assistants will pay nurse practitioners to precept students. Taking on nursing student preceptor duties alongside long working hours detracts from clinical duties at no benefit for the nurse.
Outside of paying for preceptors (a rare but effective response), schools rely on multi-tactic approaches to help their students secure placements.
Lead generation struggles complicate the picture
Though many nursing programs struggle with capacity limits, we also often hear that some programs are faced with a different challenge: a lack of qualified domestic applicants. This combined with an increase in stealth shopping behaviors and increased competition for students creates a tough environment for these programs, under immense pressure to deliver enrollments.
See How One School Met Their Enrollment Goal for Their Inaugural Nursing Cohort
One solution to this problem is expanding your lead pool by diversifying your sources. Though this can be complicated, solutions like Appily Advance help by expanding a school’s reach to source leads that nursing programs wouldn’t have found otherwise. Appily simplifies the lead generation process and deliver’s high-intent leads that align with your enrollment and program needs.
While no one silver bullet can tackle all the challenges facing nursing programs today, our EAB partners have found success using combinations of the above strategies. Increasing faculty and clinical placements allows programs to best serve student interest and meet employer demand, while diversifying lead gen sources allows programs to find the right students.

More Blogs

The big bets that actually drive online enrollment growth
How to use state demand data to launch or revitalize programs
