Addressing the need for nursing education amidst shortages
Decades of worry over the nursing shortage has only heightened during the pandemic—too few nurses have been graduating for years, and now departures (most often for retirement but also to other fields) have accelerated. Simultaneously, qualified students are turned away from nursing programs every year given capacity limitations. In 2020, over 80,000 qualified nursing school applications were rejected.
Academic leaders recognize the need for nursing education but encounter three challenges:
- The nursing shortage extends to nursing faculty, with too few instructors available to educate future nurses.
- Highly competitive clinical placements are required for graduation and licensure; however, these are hard to come by.
- Nursing is a complex field with a range of educational levels and needs, risking schools targeting the wrong opportunity for their service area.
In a June 2022 webinar, Expanding Capacity to Educate Nurses Amid Shortages and COVID-19, EAB dug into the labor market data, reviewed the literature, and talked with successful programs to identify how schools can launch and expand nursing programs. Explore the takeaways below or jump to the next steps.
Review the Key Takeaways
Faculty and clinical placement shortages prevent nursing enrollment growth despite recognized need
Demand for nurses across educational levels increased an average of 1.62% monthly from 2019 through 2021. EAB partner schools have sought to respond to this need, requesting about 30 analyses a year on launching or expanding nursing programs since 2015.
However, in that time the number of nursing programs nationwide has declined—the shortage of faculty and limited clinical placement opportunities constrains our ability to educate more nurses. Further, even once leaders overcome obstacles to growing programs, they risk misunderstanding regional nursing needs and misdirecting program resources to degree levels or qualifications unneeded in the service area.
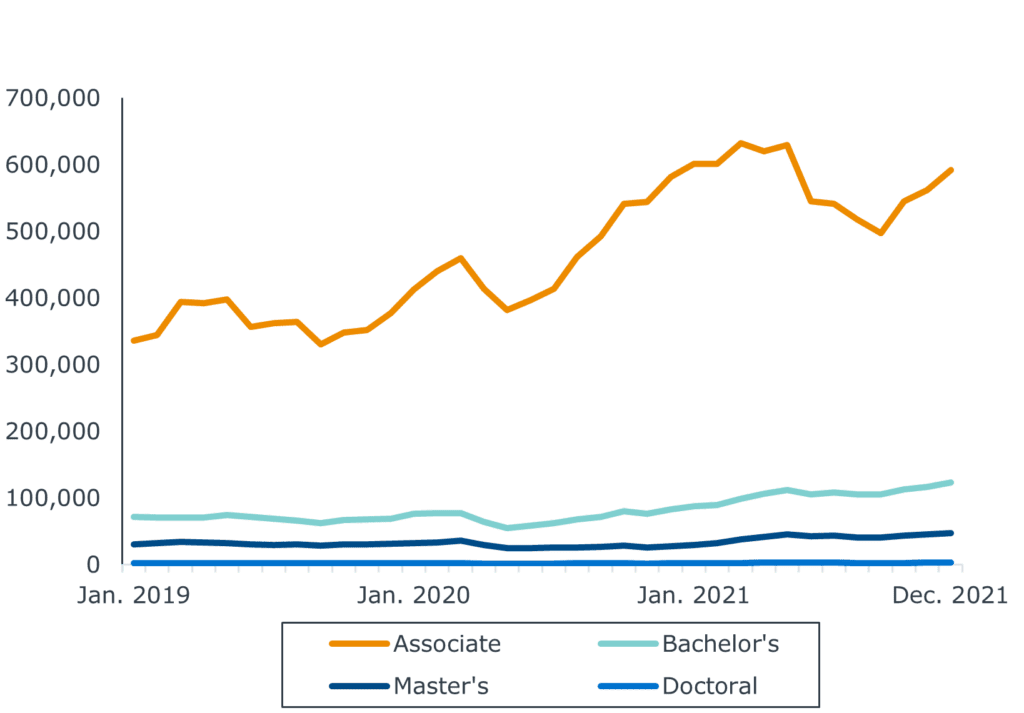
Average monthly demand growth
- Associate 1.84%
- Bachelor’s 1.77%
- Master’s 1.46%
- Doctoral 1.41%
Partner with health care providers to alleviate faculty shortage in short-term
Higher clinical salaries deter nursing professionals from pursuing faculty positions. To minimize this salary gap and attract faculty, partner with regional health care providers that can lend nursing professionals.
Schools report success with both full- and part-time partnerships. In full-time partnerships, health care providers pay their practitioners clinical rates to teach full-time. In part-time arrangements, practitioners are paid at faculty rates but the reduced number of teaching hours reduces the salary discrepancy between practice and academia.
Develop home-grown faculty to increase instructor supply long-term
Graduate-level nursing programs can tackle the faculty shortage at its root by cultivating full-time faculty from their own student bodies. Encourage existing faculty to target and support talented students showing an aptitude for teaching or research.
Ensure motivated students receive funding to support graduate-level education, whether through institutional scholarships or federal funding. Commit to hiring graduates into the faculty ranks, while remaining careful to balance “home-grown” faculty alongside external hires to maintain diversity of thought and background on campus.
Increase nonmonetary preceptor incentives and support to address clinical placement shortage
Nursing students at all degree levels must complete supervised clinical hours to earn accredited degrees. However, lack of pay and high competition makes finding preceptors increasingly difficult. Outside of paying for preceptors (a rare but effective response), nursing educators combine approaches to help their students secure placements.
Offer support systems for both preceptors and students (e.g., online guides, social media groups) and continuing education opportunities for preceptors to increase the preceptor pool with minimal costs. Replacing non-mandated hours with simulations in a lab setting or classroom also helps programs with higher clinical hour requirements provide more students with valuable experiences.
Non-financial incentives for preceptors and students
-
Preceptor support systems
Set up how-to guides, class syllabi, and social media groups to direct and support preceptors in their roles.
-
Student support systems
Offer online guides and social media groups dedicated to helping students find placements. Institutions with additional resources should employ a clinical liaison to provide personal student support.
-
Preceptor professional development incentives
Offer free or low-cost continuing education credits or certificates for participating preceptors. Institutions with limited resources can use spotlights or awards as lower-cost incentives.
-
Ongoing clinical partnerships
Setting up partnerships (ideally 3-5 years) with local acute care settings helps students gain placements while also insight into the current direction of health care and nursing.
-
Lab simulations
Replace non-mandated clinical hours with simulation options in a lab setting or classroom.
Ensure program development matches local student and employer needs
Despite widespread demand, regional variations prevent a “one size fits all” approach to nursing program development. For example, our partners shared that academic organizations and institutional leadership encourage doctoral degree development. However, labor market data indicates limited demand for doctoral-level nurses.
Carefully consider local and regional needs when developing new programs. Additionally, local and regional employers may seek skills beyond accreditation and licensure requirements such as telehealth or cultural competency. Developing electives, certificates, or alumni panels enables students to gain relevant knowledge while not detracting from accreditation- and licensure-mandated curricula.
Take the Next Steps
-
Develop recruitment messages
-
Request a program assessment
-
Share summary slides
This resource requires EAB partnership access to view.
Access the research report
Learn how you can get access to this resource as well as hands-on support from our experts through Professional and Adult Education Advisory Services.
Learn More